Premature Endemic
Even without COVID-19, wearing a mask and washing hands is a behavior that is conducive and beneficial for health. Good habits like this should be maintained and facilitated, not loosened or minimized.

Euphoria about the endemic has been circulating lately. As if the pandemic will soon end and transform into an endemic, many countries are now easing health protocols.
In France and some European countries, health protocols (prokes) have been greatly eased; even face masks are no longer needed indoors. A few days ago, Saudi Arabia lifted almost all COVID-19 restrictions, including the use of masks and verification of vaccination status when entering closed spaces.
In Indonesia, restrictions on community activities (PPKM) are still in place, but public implementation of health protocols has been very lax. The need to wear face masks and physical restrictions are starting to be ignored at the same time as the number of sporting and social events increases.
Travelers no longer need a PCR test. The government has also designed a roadmap to endemic stage, preparatory plans for entering the endemic phase. President Joko “Jokowi” Widodo has even announced relaxing the regulations to use face masks. The impression is that conditions are now improving and this country is preparing to enter an endemic phase.
Endemic is not "benign"
There are still many who think that endemic is a mild outbreak (benign outbreak) and an exit from the outbreak. Others consider it an epidemic without new cases and fatality. This assumption makes endemic status appealing. A number of countries are enthusiastic about promoting the endemic narrative. The hope is that they will get appreciation from an image of their success in overcoming the pandemic.
People are also enthusiastic; endemic is considered to be the phase that brings them back to normal life. Euphoria about endemic is massive. In fact, endemic is not a sign of the end of the epidemic or a signal that humans can live a normal life again. Endemic is a continuum of the long journey of an epidemic, not the ending. There is no guarantee that after the endemic the plague will disappear and not emerge again.
Endemic actually implies that an outbreak of disease will continue to circulate in human life; even, perhaps, for a long time. It is just that the rate of cases and deaths it causes are more stable than during the pandemic; there is no more drastic increase of cases. People are psychologically more able to accept the caseload and death without panicking.
Also read:
> Claims of Post-Truth Medical Therapy
> Facing Omicron with Vigilance without Panic
Malaria, tuberculosis and HIV/AIDS are examples of diseases that have entered an endemic phase. The case and death rates of these diseases have been relatively stable, but still high.
Every year, there are still more than 240 million cases and 600,000 deaths from malaria. Even though the magnitude is still large, people are not panicking anymore. They already have a psychological acceptance of this malaria disease.
There are currently no absolute and universal endemic metric standards. This means that there is no set of criteria that can be used as absolute standard criteria. In fact, endemic refers to a state of balance (equilibrium state) in various aspects -- health, economy, social and even political -- that can be accepted by the government and society regarding the burden of an epidemic. It is an equilibrium in which the burden of the plague is no longer considered an extreme threat and has become an accepted part of normal life. Unfortunately, there is no universal consensus about the level of burden that is acceptable to society.
Acceptance rates vary from country to country. Countries with fragile health systems may find it sufficient to use a low number of cases and deaths and high vaccination coverage as criteria for the endemic phase.
Meanwhile, countries with advanced health systems require more comprehensive criteria, such as economic and social aspects, in determining endemic status. Among parts of the consideration are the conditions and potential effects of the endemic on business activities, schools and work productivity. Roughly speaking, the criteria are more comprehensive.
Countries with fragile health systems may find it sufficient to use a low number of cases and deaths and high vaccination coverage as criteria for the endemic phase.
The World Health Organization (WHO) itself has provided a number of indicators for the transition to the endemic phase: the positivity rate must be constant below 5 percent, the virus reproduction number is below 1.0 and the coverage of the fully vaccinated population must be above 70-80 percent. There is also a criterion for the percentage of patients treated in a hospital (RS) or in an intensive care unit (ICU).
Before declaring an endemic status, countries must meet most of, if not all, the criteria. The more comprehensive the criteria that are met, the more valid and relevant a country's endemic status is. Unfortunately, this is not easy. To date, not many countries have met these comprehensive criteria. Even if they have, the profile is not constant. Several months ago, Indonesia's positivity rate was below 1 percent. Now, this positivity rate has increased to close to 10 percent.
Endemic transition
Many countries want to land quickly or give the impression that they are already entering an endemic phase. The reasons are many. They want to accommodate the pressure of the community (social mood and pressure) who are tired of the pandemic process. The endemic is also the reason and precondition for economic recovery.
The transition to the endemic phase also gives a signal that the government has successfully handled the pandemic. Because of these reasonings, many countries have actually narrated and echoed the endemic transitions. In fact, before narrating it, a very careful, wise and scientifically proven analysis is needed. Otherwise, the effect can be disastrous.
First, until now, the epidemiological profile of the pandemic has not been controlled and stable. Although at the global stage there has been a significant decrease in cases and deaths compared to during peak times, a number of countries are still struggling with up and down epidemiological profiles. Taiwan has recently experienced a significant spike in cases and deaths, whereas previously this country had success in controlling its epidemiological profile. The same thing happened in Hong Kong, Portugal and China.
Also read:
> ‘No Quarantine’ Policy Program
> Health Ethics during the Pandemic
In Indonesia, the current profile is improving although not yet fully stable. Compared to early June, the number of cases in mid-June has quadrupled with a positivity rate of 9.2 percent. In fact, a few months ago it was below 1 percent. Several other indicators are also still fluctuating. In fact, with the emergence of subvariants BA.4 and BA.5, it is predicted that there will be an additional 20,000 cases per day, the peak of which will occur in July. Given this situation, it is clear that Indonesia has not met the criteria for entering the endemic phase.
Some countries dare to relax and narrate the endemic transition based on the decline in the number of cases and deaths. In fact, endemic transition indicators are not limited to these two factors. Stability control is the keyword.
Stability itself is influenced by a number of interplays: human behavior, changes in population demographics, susceptibility, immunity and new variants. To maintain the stability of the profile, the stability of this interplay must be maintained. In addition, differences in conditions and quality of management in other countries can destabilize the epidemiological profile.
Second, the endemic phase goes hand-in-hand with a number of consequences. When the authority declares endemic status, the epidemic is no longer considered a crisis situation and there will be a degradation of commitment to it. The treatment policy will move from a centralized pattern to a decentralized one with the risk of reducing the quality and quantity of mitigation.
Funding budgets and resources will decrease. Tests and tracing will be reduced and (information) will rely on individual level without adequate data reporting. There will be many unrecorded or unreported cases (missed cases). On the other hand, people will experience endemic euphoria and underestimate COVID-19.
They will regard COVID-19 as a mild disease that is nothing more than the common cold, ignore health procedures, be reluctant to take medication if they are sick, refuse to undergo the COVID-19 vaccination and even be antipathetic to the COVID-19 management program. These factors can trigger the re-emergence of COVID-19.
Endemic delusions
Although a number of countries have implemented maximum relaxation and announced a commitment to live with the virus (live with the disease), this condition does not necessarily indicate that they have transitioned to an endemic phase. The relaxation and commitment that is echoed is more appropriate to be observed as part of the policy strategy of up and down that is commonly practiced during a pandemic. This loosening phase does not need to be prematurely coupled with issue of endemic even though from a political and social perspective, the current endemic transitional narrative is attractive.
The government must restrain and not rush to promote the narrative of the endemic transition to society. Although there is a downward trend in cases and deaths compared to some time ago, this trend has not been stable. Moreover, complete vaccination coverage of the population is still around 60 percent; it has not reached the standard of 70-80 percent as expected by WHO. Under these conditions, the epidemiological profile has the potential to change.
Also read:
> Third Wave of Pandemic, Threat or Illusion?
Cases and deaths could suddenly increase again. This risk is amplified if the community responds incorrectly to the endemic narrative and practices behavior that is not conducive to effective treatment of the situation. Echoing the narrative of endemic transition in this situation is considered by some experts as premature endemic narratives, even endemic delusions.
In addition, the government needs to be wiser and more strategic when designing relaxation policies. Standard procedures that have been practiced by the community, such as wearing masks and washing hands, should not be tampered with or relaxed. This is because this is a positive behavior that is needed not only in the prevention of COVID-19, but also in the prevention of other diseases.
Even without COVID-19, wearing a mask and washing hands is a behavior that is conducive and beneficial for health. Good habits like this should be maintained and facilitated, not loosened or minimized. The pandemic has helped to awaken these positive health behaviors. Not because the pandemic has softened, this habit is ignored again. It is like ignoring a blessing that is already in hand.
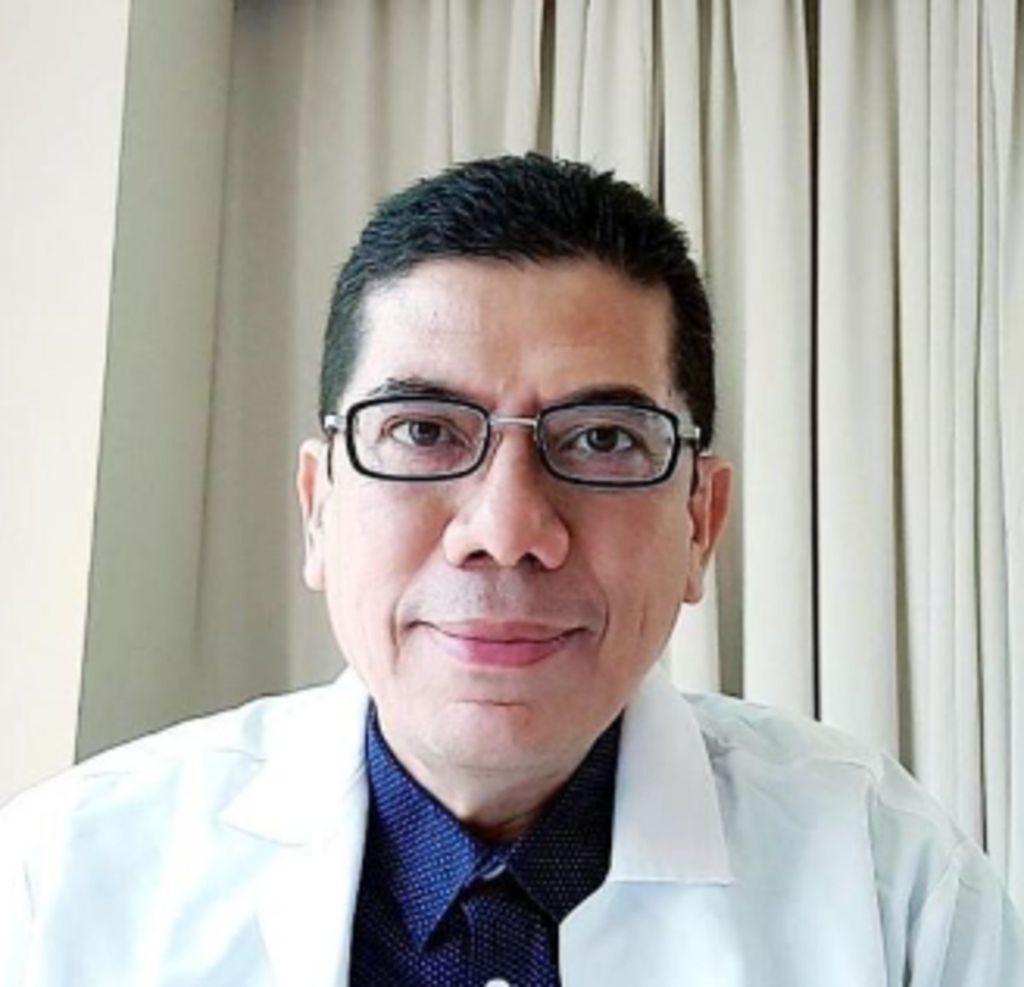
Iqbal Mochtar
Iqbal Mochtar, Physician and Doctor in Medicine and Health, Executive Member of IAKMI and PB IDI
This article was translated by Kurniawan Siswo.